Advanced renal cell carcinoma, Advanced soft tissue sarcoma
Adult: Initially, 800 mg once daily, adjust dose in 200 mg increments or decrements according to individual safety or tolerability. Max: 800 mg daily.
|
Indications and Dosage
Oral
Advanced renal cell carcinoma, Advanced soft tissue sarcoma Adult: Initially, 800 mg once daily, adjust dose in 200 mg increments or decrements according to individual safety or tolerability. Max: 800 mg daily.
|
|
Special Patient Group
Patient taking CYP3A4 inhibitors (e.g. itraconazole, clarithromycin, atazanavir, nefazodone): 400 mg once daily, may reduce dose further, as necessary.
Pharmacogenomics Pazopanib, a substrate of P-gp and BCRP, is metabolised in the liver primarily by CYP3A4 and to a minor extent by CYP1A2 and CYP2C8. It inhibits two major determinants of serum bilirubin levels, UGT1A1 and organic-anion-transporting polypeptide (OATP1B1). UGT1A1 is involved in the metabolism of bilirubin for elimination. According to studies, the inhibition of UGT1A1 activity in combination with defects of the UGT1A1 gene during pazopanib therapy may increase risk of hepatotoxicity. Other genetic variations such as human leukocyte antigen B (HLA-B) may also be associated with the development of serious liver adverse effect. However, genetic variations in OATP1B1 were not associated with bilirubin elevation related to pazopanib treatment. UGT1A1 with TA7 genotype UGT1A1 TA-repeat polymorphism is associated with hyperbilirubinaemia induced by several drugs. Patients with UGT1A1 genetic variant TA7 may have reduced UGT1A1 expression and patients with TA7/TA7 (UGT1A1 *28/*28) genotype may be predisposed to a benign form of episodic jaundice called Gilbert’s syndrome. Based on studies, the elevation of bilirubin levels during pazopanib therapy is higher in TA7/TA7 (UGT1A1 *28/*28) genotype than in TA6/TA6 and TA6/TA7 genotypes, increasing the risk of hepatotoxicity in patients with this genotype. Furthermore, similar risk is associated in patients with reduced UGT1A1 activity homozygous or heterozygous for *28, *37, *6 alleles. Researchers suggest that caution must be taken when pazopanib is used concomitantly with UGT1A1 substrates with narrow therapeutic index. Bilirubin fractionation or UGT1A1 genotyping may be considered for the safety management of the patient. HLA-B*57:01 allele According to studies, HLA alleles are associated with hepatotoxicity for several drugs (e.g. ticlopidine, flucloxacillin). In addition to risks of developing serious hepatic injury during pazopanib therapy, studies suggest that higher ALT elevation in HLA-B*57:01 allele carriers than non-carriers may indicate an immune-mediated mechanism of hepatotoxicity in some patients. Monitoring of liver function in all patients, regardless of genotype, is recommended. Genetic testing may be considered in patients with ALT elevations during treatment. |
|
Hepatic Impairment
Moderate [total bilirubin >1.5-3 x upper limit of normal (ULN)]: 200 mg once daily. Severe (total bilirubin >3 x ULN): Not recommended. Dose reduction, dosing interruption, or discontinuation may be required according to individual safety and tolerability (refer to detailed product guideline).
|
|
Administration
Should be taken on an empty stomach. Take at least 1 hr before or 2 hr after meals. Swallow whole, do not chew/crush. Avoid grapefruit juice.
|
|
Contraindications
Pregnancy and lactation. Concomitant use with other chemotherapy agents, strong P-glycoprotein (P-gp), breast cancer resistance protein (BCRP); strong CYP3A4 inducers, and agents which increase gastric pH (e.g. PPI, H2 antagonists).
|
|
Special Precautions
Patient with history of QT interval prolongation, pre-existing cardiac disease, risk factors or history of thrombotic events, risk of haemorrhage, GI perforation or fistula. Renal and mild to moderate hepatic impairment. Elderly. Patient with genetic variation of UGT1A1 TA7 genotype and HLA-B*57:01 allele. Concomitant use with strong CYP3A4 inhibitors. Discontinue treatment 7 days prior to surgery and in patients with wound dehiscence.
|
|
Adverse Reactions
Significant: Hypertension (including hypertensive crisis), cardiac dysfunction (e.g. CHF, decreased LVEF), QT prolongation, torsade de pointes, venous thrombosis, thrombotic microangiopathy (TMA) including thrombotic thrombocytopenic purpura, hemolytic uremic syndrome; retinal tear/detachment, hand-foot skin reaction, hypothyroidism, proteinuria, pneumothorax.
Blood and lymphatic system disorders: Thrombocytopenia, neutropenia, leukopenia, polycythemia. Cardiac disorders: Bradycardia, chest pain. Eye disorders: Blurred vision, retinal detachment or tear. Gastrointestinal disorders: Diarrhoea, anorexia, dysgeusia, nausea, vomiting, abdominal pain, stomatitis, dyspepsia, flatulence. General disorders and admin site conditions: Fatigue, mucosal inflammation, asthenia, hyperhidrosis, lethargy, chills. Hepatobiliary disorders: Pancreatitis. Investigations: Increased LFT, creatinine, lipase, thyroid-stimulating hormone, blood glucose; weight decreased. Metabolism and nutrition disorders: Decreased appetite, oedema. Musculoskeletal and connective tissue disorders: Arthralgia, myalgia, muscle spasms, musculoskeletal pain. Neoplasms benign, malignant and unspecified: Tumour pain. Nervous system disorders: Headache, dysgeusia, dizziness, paraesthesia, peripheral sensory neuropathy. Psychiatric disorders: Insomnia. Respiratory, thoracic and mediastinal disorders: Dysphonia, cough, dyspnoea, hiccups. Skin and subcutaneous tissue disorders: Hair colour change, palmar-plantar erythrodysaesthesia syndrome, alopecia, exfoliative rash, hypopigmentation, dry skin, pruritus, erythema, depigmentation, nail disorder. Potentially Fatal: Interstitial lung disease/pneumonitis, arterial thrombotic events (e.g. MI, myocardial ischaemia, ischaemic stroke, transient ischaemic attacks), haemorrhage (e.g. epistaxis, haemoptysis, rectal or anal haemorrhage, mouth haemorrhage), pulmonary embolism, serious infections (with or without neutropenia), gastrointestinal perforation or fistula. Rarely, reversible posterior leukoencephalopathy syndrome (e.g. headache, seizure, lethargy). |
|
Patient Counseling Information
This drug may cause dizziness, tiredness and weakness, if affected, do not drive or operate machinery.
|
|
Monitoring Parameters
Monitor LFT (e.g. ALT, AST, bilirubin), BP, serum electrolytes (e.g. Ca, Mg, K), ECG and thyroid function (e.g. TSH, T4) prior to and during therapy. Monitor signs and symptoms of infection, neurological changes (e.g. confusion, visual disturbances, lethargy), gastrointestinal perforation or fistula, pulmonary conditions indicative of pneumonitis, venous or arterial thrombotic events, and heart failure.
|
|
Overdosage
Symptoms: Grade 3 fatigue and hypertension. Management: Supportive treatment.
|
|
Drug Interactions
Increased plasma concentration of midazolam, dextromethorphan (metabolites), and paclitaxel. Increased plasma concentration of uridine diphosphoglucuronosyl-transferase 1A1 (UGT1A1) substrates (e.g. irinotecan). Increased ALT levels with simvastatin. Increased risk of QT interval prolongation with concomitant use of QT-prolonging agents (e.g. haloperidol, lapatinib).
Potentially Fatal: Increased risk of toxicity (e.g. pulmonary haemorrhage, gastrointestinal haemorrhage) and/or mortality with concomitant use of pemetrexed and lapatinib. Increased serum concentration with strong inhibitors of CYP3A4 (e.g. itraconazole, clarithromycin, atazanavir, nefazodone, lapatanib), P-gp, and BCRP. Decreased serum concentration with CYP3A4 inducers (e.g. rifampin), PPI (e.g. esomeprazole). |
|
Food Interaction
Increased system exposure with food. Avoid use with grapefruit or grapefruit juice as it increases serum concentration with food. Decreased serum concentration with St John’s wort.
|
|
Action
Description: Pazopanib is an inhibitor of multiple receptor tyrosine kinases (RTKs) which are involved in the initiation of signal transduction pathways that lead to proliferation of malignant cells and affect processes critical to cell survival and tumour progression. RTKs involved in the blockade include receptors for vascular endothelial growth factors (VEGFR-1, -2, and -3), platelet-derived growth factors (PDGFR-α and -β), fibroblast growth factor receptor (FGFR-1 and -3), stem cell factor [e.g. cytokine receptor (cKIT)], interleukin-2 receptor inducible T-cell kinase, lymphocyte-specific protein tyrosine kinase (Lck), and transmembrane glyocoprotein receptor tyrosine kinase (c-Fms).
Pharmacokinetics: Absorption: Increased systemic exposure with food. Time to peak plasma concentration: Approx 2-4 hours. Distribution: Plasma protein binding: >99%. Metabolism: Metabolised in the liver mainly by CYP3A4 and to a minor extent by CYP1A2 and CYP2C8. Excretion: Mainly via faeces, urine (<4%). Elimination half-life: Approx 31 hours. |
|
Chemical Structure
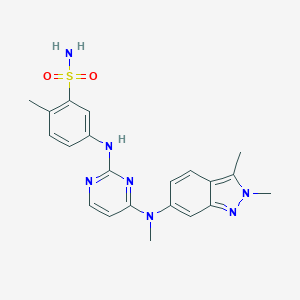 Source: National Center for Biotechnology Information. PubChem Database. Pazopanib, CID=10113978, https://pubchem.ncbi.nlm.nih.gov/compound/Pazopanib (accessed on Jan. 22, 2020) |
|
Storage
Store between 20-25°C. This is a cytotoxic drug. Any unused portion should be disposed of in accordance with local requirements.
|
|
MIMS Class
|
|
ATC Classification
L01EX03 - pazopanib ; Belongs to the class of other protein kinase inhibitors. Used in the treatment of cancer.
|
|
References
Motzer R.J., Johnson T, Choueiri T. K., et al. Hyperbilirubinemia in pazopanib- or sunitinib-treated patients in COMPARZ is associated with UGT1A1 polymorphisms. Annals of Oncology: Official Journal of the European Society for Medical Oncology. 2013 Nov;24(11):2927-2928. doi: 10.1093/annonc/mdt394. Accessed 06/08/2019. PMID: 24107802 Xu C-F, Johnson T, Wang X et al. HLA-B*57:01 Confers Susceptibility to Pazopanib-Associated Liver Injury in Patients with Cancer. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2016 Mar;22(6):1371-7. doi: 10.1158/1078-0432.CCR-15-2044. Accessed 07/08/2019. PMID: 26546620 Xu, C-F, Reck B, Xue Z et al. Pazopanib-induced hyperbilirubinemia is associated with Gilbert's syndrome UGT1A1 polymorphism. British Journal of Cancer. 2010 Apr;102(9):1371-1377. doi: 10.1038/sj.bjc.6605653. Accessed 06/08/2019. PMID: 20389299 Annotation of EMA Label for Pazopanib and HLA-B. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 07/08/2019. Annotation of FDA Label for Pazopanib and HLA-B, UGT1A1. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 07/08/2019. Anon. Pazopanib. Lexicomp Online. Hudson, Ohio. Wolters Kluwer Clinical Drug Information, Inc. https://online.lexi.com. Accessed 05/08/2019. Buckingham R (ed). Pazopanib Hydrochloride. Martindale: The Complete Drug Reference [online]. London. Pharmaceutical Press. https://www.medicinescomplete.com. Accessed 05/08/2019. Pazopanib. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 07/08/2019. Votrient Tablet (Novartis Europharm Limited). European Medicines Agency [online]. Accessed 06/08/2019. Votrient Tablet (Novartis Pharmaceuticals Corporation). U.S. FDA. https://www.fda.gov/. Accessed 06/08/2019. Votrient Tablet, Film Coated (Novartis Pharmaceuticals Corporation). DailyMed. Source: U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/. Accessed 05/08/2019.
|