Tardive dyskinesia
Adult: Initially, 40 mg once daily for 1 week, increased to 80 mg once daily. Consider continuation of 40 mg once daily dose based on patient response and tolerability.
|
Indications and Dosage
Oral
Tardive dyskinesia Adult: Initially, 40 mg once daily for 1 week, increased to 80 mg once daily. Consider continuation of 40 mg once daily dose based on patient response and tolerability.
|
||||
|
Special Patient Group
Patients taking strong CYP3A4 inhibitors (e.g. itraconazole, ketoconazole, clarithromycin): Reduce maintenance dose to 40 mg once daily.
Patients taking strong CYP3A4 inducers (e.g. carbamazepine, phenytoin, rifampicin): Not recommended. Patients taking strong CYP2D6 inhibitors (e.g. paroxetine, fluoxetine, quinidine): Consider dose reduction based on patient tolerability. Pharmacogenomics: Valbenazine is metabolised to its active metabolite, (+)-α-HTBZ, via hydrolysis of valine ester. (+)-α-HTBZ is further metabolised in part by CYP2D6. Patients who are CYP2D6 poor metabolisers or concomitantly taking strong CYP2D6 inhibitors may have increased serum concentrations of valbenazine and (+)-α-HTBZ active metabolite thereby may increase risk of adverse effects (e.g. QT prolongation). The FDA-approved drug label recommends considering dose reduction for patients who are known CYP2D6 poor metabolisers based on tolerability. |
||||
|
Renal Impairment
|
||||
|
Hepatic Impairment
Moderate to severe (Child-Pugh score 7-15): 40 mg once daily.
|
||||
|
Administration
cap: May be taken with or without food.
|
||||
|
Contraindications
Patients with congenital long QT syndrome or arrhythmias associated with prolonged QT interval. Concomitant use with MAOIs (e.g. isocarboxazid, phenelzine, selegiline).
|
||||
|
Special Precautions
CYP2D6 poor metabolisers. Severe renal and moderate to severe hepatic impairment. Pregnancy and lactation.
|
||||
|
Adverse Reactions
Significant: Prolonged QT interval, Parkinson-like symptoms (e.g. falls, gait disturbances, tremor, drooling, hypokinesia), somnolence, hypersensitivity reactions (e.g. allergic dermatitis, angioedema, pruritus, urticaria).
Eye disorders: Blurred vision. Gastrointestinal disorders: Dry mouth, constipation, vomiting, nausea. General disorders and administration site conditions: Fatigue, balance disorder. Investigations: Increased blood glucose, increased weight. Musculoskeletal and connective tissue disorders: Arthralgia. Nervous system disorders: Sedation, dyskinesia, dizziness, headache, extrapyramidal symptoms (non-akathisia). Psychiatric disorders: Akathisia, restlessness, anxiety, insomnia, disturbance in attention. Renal and urinary disorders: Urinary retention. Respiratory, thoracic and mediastinal disorders: Respiratory infections. |
||||
|
Patient Counseling Information
This drug may cause somnolence, if affected, do not drive or operate machinery.
|
||||
|
Monitoring Parameters
Monitor for signs of involuntary movement or Parkinson-like symptoms. Perform ECG prior to increasing dose in patient at risk of QT prolongation.
|
||||
|
Drug Interactions
Increased risk of adverse effects with strong inhibitors of CYP2D6 (e.g. paroxetine, fluoxetine, quinidine) or CYP3A4 (e.g. itraconazole, ketoconazole, clarithromycin). May reduce efficacy of valbenazine with strong CYP3A4 inducers (e.g. rifampicin, carbamazepine, phenytoin). Increased serum concentration of P-glycoprotein substrates (e.g. digoxin).
Potentially Fatal: Increased risk of adverse effects (e.g. serotonin syndrome) of MAOIs (e.g. isocarboxazid, phenelzine, selegiline). |
||||
|
Food Interaction
Decreased serum concentrations of valbenazine with St. John’s wort and high-fat food.
|
||||
|
Action
Description: Valbenazine reversibly inhibits the vesicular monoamine transporter 2 (VMAT2) which regulates the uptake of monoamine from the cytoplasm to the synaptic vesicle for storage and release. It has no binding affinity for VMAT1 nor the dopaminergic, serotonergic, adrenergic, histaminergic or muscarinic receptors.
Pharmacokinetics: Absorption: Bioavailability: Approx 49%. Time to peak plasma concentrations: 0.5-1 hour (valbenazine); 4-8 hours (active metabolite). Decreased serum concentration with high fat meal. Distribution: Volume of distribution: 92 L. Plasma protein binding: >99% (valbenazine); approx 64% (active metabolite). Metabolism: Extensively metabolised via hydrolysis of valine ester to active metabolite, (+)-α-dihydroxytetrabenazine [(+)-α-HTBZ] and via oxidative metabolism by CYP3A4/5 to mono-oxidised valbenazine and other minor metabolites. (+)-α-HTBZ is further metabolised in part by CYP2D6. Excretion: Via urine (approx 60%, mainly as inactive metabolites; <2% as unchanged drug or active metabolite); via faeces (30%, mainly as inactive metabolites; <2% as unchanged drug or active metabolite). Elimination half-life: 15-22 hours. |
||||
|
Chemical Structure
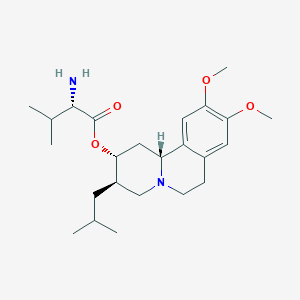 Source: National Center for Biotechnology Information. PubChem Database. Valbenazine, CID=24795069, https://pubchem.ncbi.nlm.nih.gov/compound/Valbenazine (accessed on Jan. 23, 2020) |
||||
|
Storage
Store below 30°C.
|
||||
|
MIMS Class
|
||||
|
ATC Classification
N07XX13 - valbenazine ; Belongs to the class of other nervous system drugs.
|
||||
|
References
Uhlyar S, Rey JA. Valbenazine (Ingrezza): The First FDA-Approved Treatment for Tardive Dyskinesia. Drug Forecast. 2018 Jun;43(6):328-331. Accessed 17/10/2019 Annotation of FDA Label for Valbenazine and CYP2D6. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 17/10/2019. Anon. Valbenazine. Lexicomp Online. Hudson, Ohio. Wolters Kluwer Clinical Drug Information, Inc. https://online.lexi.com. Accessed 17/10/2019. Buckingham R (ed). Valbenazine. Martindale: The Complete Drug Reference [online]. London. Pharmaceutical Press. https://www.medicinescomplete.com. Accessed 17/10/2019. Ingrezza (Neurocrine Biosciences, Inc.). DailyMed. Source: U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/. Accessed 17/10/2019. Ingrezza (Neurocrine Biosciences, Inc.). U.S. FDA. https://www.fda.gov/. Accessed 17/10/2019.
|