Hypertensive crisis
Adult: 10-20 mg as a single dose, a further dose of 10-20 mg may be given after 3 hours, if necessary.
|
Indications and Dosage
Intramuscular
Hypertensive crisis Adult: 10-20 mg as a single dose, a further dose of 10-20 mg may be given after 3 hours, if necessary.
|
||||||
|
Renal Impairment
|
||||||
|
Contraindications
Phaeochromocytoma, heart failure unrelated to hypertension. Concomitant use or within 2 weeks of MAOIs. Severe renal impairment (CrCl 10-40 mL/min).
|
||||||
|
Special Precautions
Patient with coronary or cerebral artery disease, asthma, history of gastrointestinal ulceration, Parkinson’s disease with associated autonomic neuropathy. Moderate renal impairment (CrCl 41-65 mL/min). Pregnancy (not recommended during the 1st trimester or within 2 weeks before labour) and lactation. Withdraw treatment few days prior to surgery.
|
||||||
|
Adverse Reactions
Significant: CNS effect (e.g. dizziness, blurred vision, drowsiness), latent heart failure (prolonged use), fever.
Cardiac disorders: Bradycardia, sick-sinus syndrome. Gastrointestinal disorders: Nausea, diarrhoea, vomiting, dry mouth, gaseous distension. General disorders and administration site conditions: Lethargy, oedema, tiredness. Investigations: Increased BUN levels (in patients with latent or manifest renal failure). Nervous system disorders: Headache, paraesthesia. Renal and urinary disorders: Uraemia (in patients with latent or manifest renal failure). Reproductive system and breast disorders: Ejaculation disturbances, erectile dysfunction (including priapism). Respiratory, thoracic and mediastinal disorders: Rarely, asthma. Vascular disorders: Postural hypotension, exacerbation of intermittent claudication. |
||||||
|
Patient Counseling Information
This drug may cause dizziness, drowsiness, or blurred vision, if affected, do not drive or operate machinery.
|
||||||
|
Monitoring Parameters
Monitor blood pressure and renal function.
|
||||||
|
Overdosage
Symptoms: Postural hypotension causing syncope, sinus bradycardia, tiredness, dizziness, tachycardia, blurred vision, muscle weakness, nausea, vomiting, severe diarrhoea, and oliguria. Management: Symptomatic treatment. In case of postural hypotension, keep the patient in a recumbent position or institute fluid and electrolyte replacement; if necessary, may administer pressor agents. Administer atropine for sinus bradycardia. Treat diarrhoea with an anticholinergic agent.
|
||||||
|
Drug Interactions
May lead to sinus bradycardia when given concurrently with antiarrhythmic agents and digitalis. Antihypertensive effect may be increased by reserpine, methyldopa, vasodilators (e.g. minoxidil), calcium channel blockers, β-blockers, ACE inhibitors. Antihypertensive effect may be decreased by TCAs, phenothiazine derivatives, chlorpromazine, oral contraceptives. May increase hypersensitivity to adrenaline, amphetamines, or other sympathomimetic agents.
Potentially Fatal: May lead to release of large quantities of catecholamines causing hypertensive crisis when given to patient previously treated with MAOIs. |
||||||
|
Food Interaction
Alcohol may enhance the antihypertensive effect of guanethidine.
|
||||||
|
Action
Description: Guanethidine is a peripheral sympathetic blocking agent. It lowers blood pressure by depleting and inhibiting reformation of noradrenaline in postganglionic nerve endings, but it does not prevent the secretion of catecholamines by the adrenal medulla.
Onset: Fall in blood pressure: Within 30 minutes. Pharmacokinetics: Distribution: Enters breast milk (small amounts). Metabolism: Partially metabolised in the liver. Excretion: Via urine as metabolites and unchanged drug. Terminal half-life: Approx 5 days. |
||||||
|
Chemical Structure
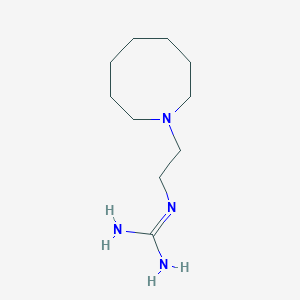 Source: National Center for Biotechnology Information. PubChem Compound Summary for CID 3518, Guanethidine. https://pubchem.ncbi.nlm.nih.gov/compound/Guanethidine. Accessed Mar. 25, 2021. |
||||||
|
MIMS Class
|
||||||
|
ATC Classification
C02CC02 - guanethidine ; Belongs to the class of guanidine derivatives, peripherally-acting antiadrenergic agents. Used in the treatment of hypertension.
|
||||||
|
References
Anon. Guanethidine. Lexicomp Online. Hudson, Ohio. Wolters Kluwer Clinical Drug Information, Inc. https://online.lexi.com. Accessed 09/03/2021. Buckingham R (ed). Guanethidine Monosulfate. Martindale: The Complete Drug Reference [online]. London. Pharmaceutical Press. https://www.medicinescomplete.com. Accessed 09/03/2021. Ismelin 10 mg/mL Ampoules (Amdipharm UK Limited). MHRA. https://products.mhra.gov.uk. Accessed 09/03/2021.
|